Marijuana-induced psychosis is a serious mental health condition that can occur when using cannabis, particularly high-potency products. When someone experiences cannabis-induced psychosis, they temporarily lose touch with reality in ways that can be frightening and dangerous.
This condition represents one of the more severe adverse reactions to cannabis use and can occur unexpectedly, even in individuals who have previously used cannabis without incident. The psychological break from reality typically involves a combination of perceptual disturbances and disordered thinking patterns that significantly impair a person’s ability to function normally and safely interact with their environment.
How Does Cannabis-Induced Psychosis Feel?
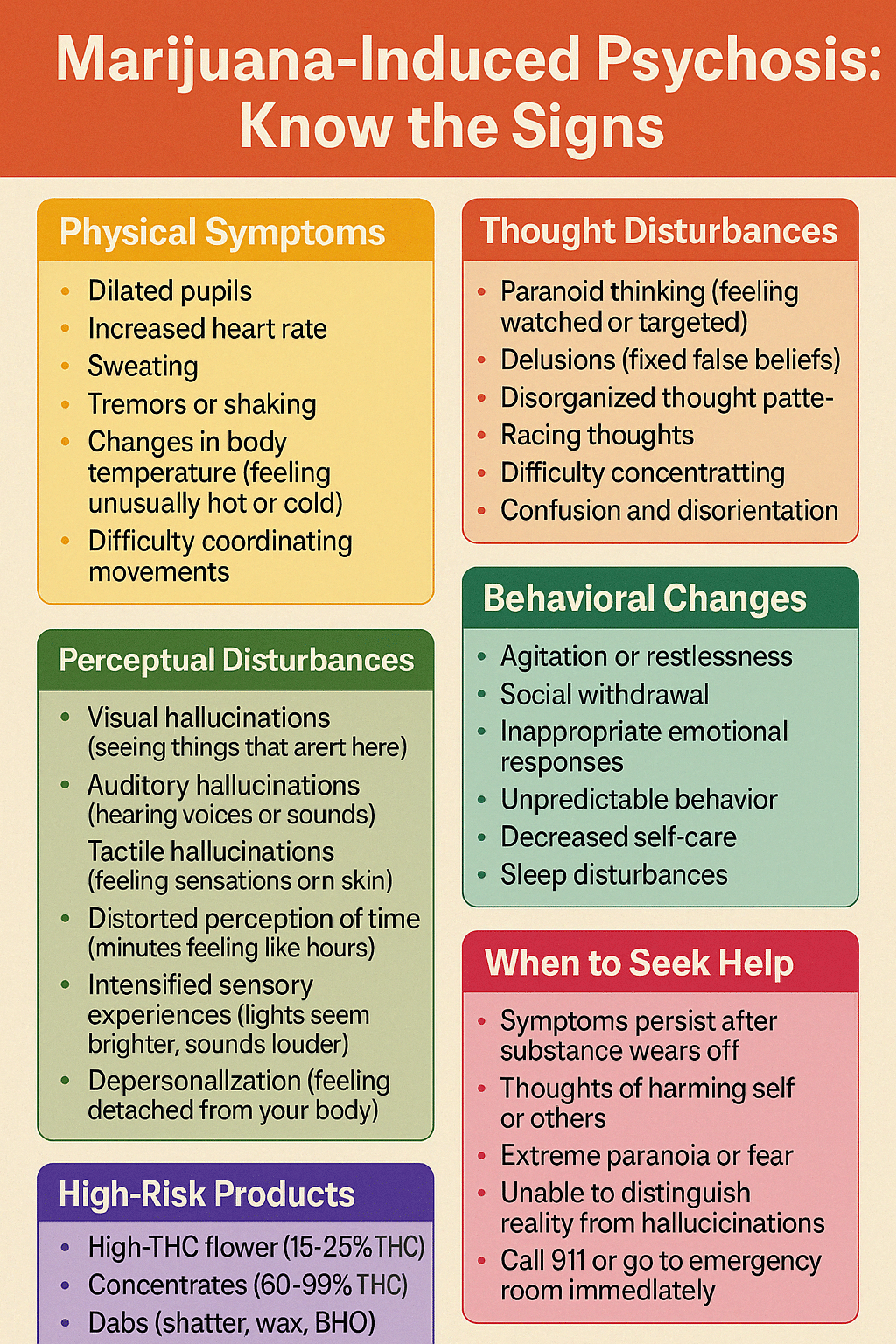
During an episode of marijuana-induced psychosis, an individual may experience hallucinations where they perceive things that aren’t actually present, such as seeing shapes or figures, hearing voices or sounds, or feeling sensations on their skin with no external cause. Delusions often accompany these hallucinations, where the person develops fixed, false beliefs that cannot be changed with logical reasoning or evidence.
Many people experiencing cannabis-induced psychosis develop intense paranoia, becoming irrationally suspicious of friends, family members, or even strangers. The cognitive disruption typically includes disorganized thinking patterns where thoughts become fragmented and difficult to follow, leading to confused speech and behavior.
This often accompanies a profound sense of disorientation, where the person may not understand where they are or what’s happening around them. Throughout this experience, extreme anxiety or panic frequently intensifies the distress, creating a terrifying mental state that can lead to unpredictable behaviors.
Who Can Experience Cannabis-Induced Psychosis?
Although many cannabis users never experience psychosis, it’s crucial to understand that the risk is real and significant for certain individuals. Modern cannabis products with high THC concentrations have been associated with increased rates of psychotic episodes compared to the lower-potency cannabis of previous generations. For some vulnerable individuals, psychotic symptoms can emerge after a single use, particularly with high-potency concentrates or edibles. However, the risk generally increases with regular, heavy use of products with high THC content and minimal CBD, a cannabinoid that may offer some protective effects against THC’s psychoactive properties. Learn more about marijuana psychosis and the risk of developing schizophrenia on our blog.
According to the National Institute on Drug Abuse (NIDA), research has linked cannabis use with “an increased likelihood of developing head, neck, or throat cancer” and “some evidence has linked cannabis use to earlier onset of psychosis in people with genetic risk factors for psychotic disorders” (NIDA, 2024).
The Cannabis Potency Revolution:
Not Your Parents' Marijuana
The cannabis landscape has transformed dramatically over recent decades, with today’s marijuana bearing little resemblance to what previous generations consumed. This evolution in potency represents one of the most significant yet underappreciated changes in modern drug use patterns.
Through intensive selective breeding programs and advanced cultivation techniques, cannabis producers have systematically increased the THC content of their products while often reducing CBD levels, creating products optimized for maximum psychoactive effect rather than balanced therapeutic benefit.
How Has Cannabis Potency Changed Over Time?
In the 1970s, the average THC content in cannabis samples was approximately 2%, creating a relatively mild psychoactive experience by today’s standards. Most cannabis available during this era was imported as less potent mixtures of leaves, stems, and flowers.
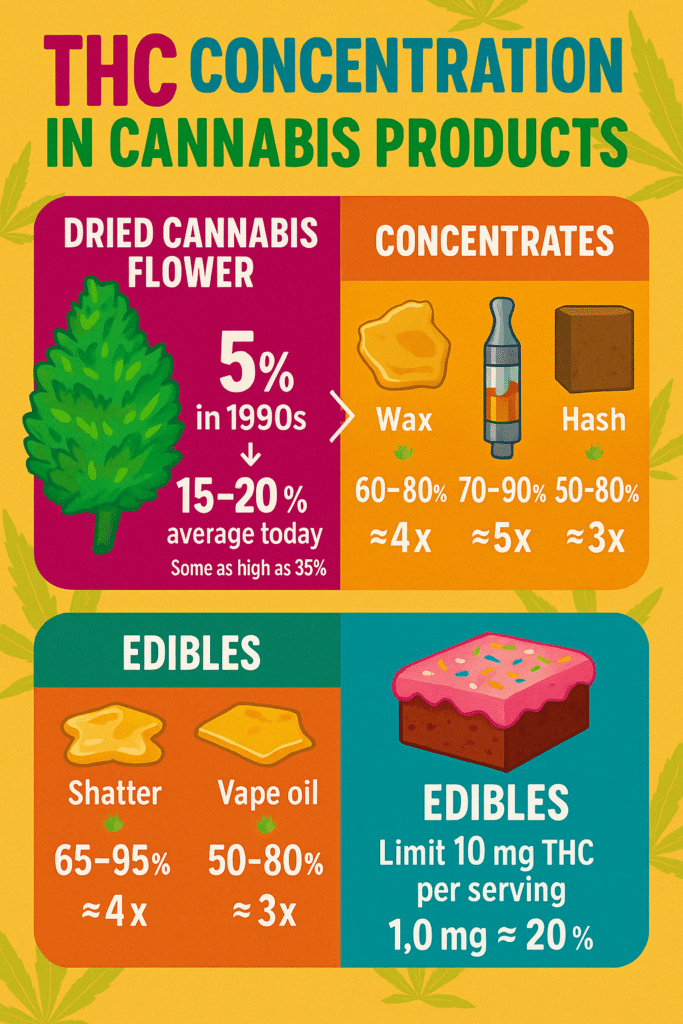
By the 1990s, as domestic cultivation increased and growing techniques improved, average THC concentrations had doubled to around 4-5%, still modest compared to current products. Today’s commercially grown cannabis flowers regularly test between 15-25% THC, representing a five to ten-fold increase over what was available just a few decades ago. This dramatic escalation continues with modern concentrates, which can range from 40% to nearly pure THC at 99%, creating products with unprecedented potency in human history.
According to research published by the National Institutes of Health, “the mean Δ9-THC concentration has increased over the last 10 years, from 9.75% in 2009 to 14.88% in 2018 and 13.88% in 2019” (ElSohly et al., 2021). NIDA reports that “between 1995 and 2022 the delta-9 THC potency (strength) in illegal cannabis products seized by law enforcement quadrupled from 3.96% to 16.14%” (NIDA, 2024).
Why Does the Potency Revolution Matter?
This revolution in cannabis potency has profound implications for public health and safety. The human endocannabinoid system, which THC directly impacts, was never evolutionarily prepared to handle such concentrated exposures. Research increasingly suggests that the substantial rise in cannabis-related emergency room visits, including those for psychosis, correlates directly with this increase in potency.
When discussing cannabis today, it’s critical to recognize that we’re effectively talking about a different substance than what previous generations used, with different risk profiles and potential consequences, particularly regarding mental health outcomes.
A comprehensive study from the NIH has found that “young men with cannabis (marijuana) use disorder have an increased risk of developing schizophrenia” and statistical models estimated that “as many as 30% of cases of schizophrenia among men aged 21-30 might have been prevented by averting cannabis use disorder” (NIH, 2023).
The Concentration Factor:
Breaking Down Cannabis Products by Potency
Understanding the varying THC concentrations across different cannabis products is essential for accurately assessing potential risks and making informed decisions about consumption. The type of cannabis product used significantly influences both the intensity and nature of effects experienced, with higher concentrations generally associated with greater risk of adverse psychological reactions, including psychosis.
Traditional Flower: Lower Risk, But Not Risk-Free
Traditional cannabis flower remains the most recognizable form of marijuana, though even this “natural” product has changed substantially. Today’s cannabis buds typically contain between 15-25% THC, significantly higher than historical averages due to sophisticated breeding and cultivation techniques.
While this represents the least concentrated form of cannabis currently available in most markets, today’s flower is still potent enough to trigger adverse reactions in sensitive individuals, especially when consumed in large amounts. Even experienced cannabis users from previous generations may be unprepared for the potency of modern flower products, which can deliver effects far more intense than anticipated.
Research published in the U.S. National Library of Medicine has found that “the majority of products, regardless of medicinal or recreational programs, were advertised to have >15% THC (70.3% – 91.4% of products)” which seems “unsuitable for medicinal purposes, particularly for patients with chronic neuropathic pain” (Cash et al., 2020).
Mid-Range Concentrates: Hash and Traditional Extracts
Hash and traditional concentrates represent an intermediate level of potency, typically ranging from 20-60% THC. These products condense the resin glands of the cannabis plant where cannabinoids are most concentrated.
Traditional hash has been used for centuries in various cultures, but modern production methods have increased potency. The risk level with these products increases proportionally with their concentration, creating a moderate to high risk of adverse effects, including psychotic symptoms in vulnerable individuals.
High-Risk Products: Vape Cartridges and Their Unique Concerns
Vape cartridges have revolutionized cannabis consumption with their convenience and discretion, but they typically contain highly concentrated cannabis oils ranging from 60-90% THC. The rapid delivery method of vaporization allows THC to reach the brain quickly, potentially intensifying its effects.
The ease of use and minimal odor can lead to more frequent consumption and higher overall THC intake, creating patterns of use that substantially increase risk. The temperature and other aspects of vaporization may also affect the risk profile of these products in ways that are still being studied. For more information on vaping and its risks, see our article on what drugs can be vaped.
Extreme Potency: Why Are Dabs So Dangerous?
Dabs—including products known as shatter, wax, budder, and butane hash oil (BHO)—represent the highest concentration of cannabis products widely available today. These extracts can contain between 60-99% THC, approaching pharmaceutical-grade purity. Even a single use of these ultra-potent concentrates can deliver more THC than multiple sessions with traditional flower.
The extreme potency of these products creates a very high risk profile, with increased reports of anxiety, paranoia, and psychotic reactions even among experienced cannabis users with established tolerance. The rapid onset and intensity of effects can overwhelm the brain’s ability to process the experience, potentially triggering acute psychiatric emergencies.
According to Yale Medicine, “we now have concentrated THC products such as oil, shatter, dab, and edibles that have been able to get the THC concentration upwards of 95%” and “there is absolutely no research that indicates this level of THC is beneficial for any medical condition” (Stuyt, 2019).
Why Are Edibles Particularly Tricky?
Edibles present unique risks due to their delayed onset and prolonged effects. While THC content varies dramatically from 5mg in single servings to over 1000mg in some packages, the critical factor with edibles is how THC is metabolized. When consumed orally, the liver converts THC to 11-hydroxy-THC, a metabolite that crosses the blood-brain barrier more efficiently and produces stronger psychoactive effects than inhaled THC.
This distinctive pharmacokinetic profile, combined with the typical delay of 30-90 minutes before effects begin, frequently leads to overconsumption as impatient users take additional doses before feeling the full effects of their initial dose. This pattern creates a particularly high risk for unexpected and severe adverse reactions, including intense and prolonged psychotic episodes.
Who is Most Vulnerable to Cannabis-Induced Psychosis?
Cannabis affects each person differently, and while psychotic reactions are relatively rare in the general population, certain biological, psychological, and environmental factors significantly increase vulnerability. Understanding these risk factors can help individuals make more informed decisions about cannabis use based on their personal risk profile.
How Do Genetics Influence Cannabis Psychosis Risk?
Genetic predisposition plays a crucial role in determining vulnerability to cannabis-induced psychosis. Individuals with a family history of psychotic disorders such as schizophrenia or bipolar disorder, carry a substantially higher risk, as cannabis use can potentially trigger latent psychological conditions. Research has identified specific genetic variations that affect how the brain responds to cannabinoids, potentially explaining why some people experience psychosis while others using identical products do not.
These genetic factors influence both the endocannabinoid system and dopamine regulation, key neurological systems involved in psychosis development. If close biological relatives have experienced psychotic disorders, the risk of cannabis triggering similar conditions increases significantly.
According to research published in Psychological Medicine, “The entanglement of substance use disorders and mental illnesses is a major public health issue, requiring urgent action and support for people who need it,” and studies show that “early, frequent cannabis use is associated with an increased risk of developing schizophrenia” (NIH, 2023).
Mental Health and Cannabis: A Complicated Relationship
A personal history of mental health conditions also dramatically elevates the risk of experiencing cannabis-induced psychosis. Pre-existing conditions such as anxiety disorders, depression, bipolar disorder, or previous psychotic episodes create neurological vulnerabilities that cannabis can exacerbate. Even subclinical symptoms or personality traits like schizotypy (having thoughts and behaviors similar to but less severe than schizophrenia) can indicate increased risk.
The self-medication hypothesis suggests that many individuals with undiagnosed mental health conditions may be drawn to cannabis use to manage their symptoms, ironically increasing their risk of more serious psychological complications. Our article on the connection between anxiety and addiction explores these relationships in greater depth.
Research from the National Institutes of Health shows that “cannabis-induced psychosis could be an early sign of schizophrenia rather than a distinct clinical entity” and that “cannabinoids can induce transient schizophrenia-like positive, negative, and cognitive symptoms, and exacerbate symptoms in schizophrenic patients” (D’Souza et al., 2009).
Why Are Young People at Greater Risk?
Age represents another critical factor, with adolescents and young adults showing particularly high vulnerability. The human brain continues developing until approximately age 25, with the prefrontal cortex, responsible for judgment, decision-making, and impulse control—being one of the last regions to fully mature. Cannabis use during this critical developmental period appears to interfere with normal neurodevelopmental processes and potentially alter brain structure and function.
Research consistently shows that early cannabis use carries higher risks for both immediate psychotic reactions and the subsequent development of chronic psychotic disorders. The risk appears dose-dependent, with heavier use, earlier onset of use, and higher potency products all associated with greater risk for young users. Learn more about signs of teen drug abuse to identify potential problems early.
The National Institute on Drug Abuse states that “cannabis use at a young age has also been linked to other mental health conditions, including the likelihood of developing psychosis” and that they are conducting the ABCD Study® to explore “the effects of environmental, social, genetic, and other biological factors on the developing adolescent brain” (NIDA, 2024).
Warning Signs to Watch For
Recognizing the early warning signs of cannabis-induced psychosis can potentially prevent a full psychotic episode and ensure timely intervention. Cannabis affects the brain’s endocannabinoid system, which plays important roles in mood regulation, perception, and cognitive function.
When this system becomes severely dysregulated through high-dose or high-potency cannabis use, subtle psychological changes often precede more severe symptoms. These warning signs may develop gradually over time or appear suddenly, particularly with high-dose exposure.
What Are the Early Warning Signs of Cannabis Psychosis?
Increasing paranoia or suspiciousness often represents one of the earliest warning signs of impending psychosis. A person may begin expressing concerns about being watched, followed, or targeted by others without reasonable evidence.
This paranoia might initially focus on strangers but can eventually extend to friends and family members. Perceptual disturbances like hearing voices or experiencing visual hallucinations indicate a significant disruption in normal brain function. These might begin subtly—misinterpreting normal sounds or seeing movement in peripheral vision—before progressing to more defined hallucinations. The content of these perceptions often reflects underlying anxiety or paranoia.
Research from the U.S. National Library of Medicine shows that “Cannabis intoxication can lead to acute psychosis in many individuals and can produce short-term exacerbations of pre-existing psychotic diseases” and that reported symptoms include “depersonalization, fear of dying, irrational panic, and paranoid ideas” (Khan et al., 2012).
How Does Behavior Change Before a Full Psychotic Episode?
As cannabis-induced psychosis develops, individuals typically begin expressing unusual or bizarre beliefs that represent significant departures from their previous thinking patterns or cultural context. These might include ideas about special powers, conspiracies, or messages being communicated through ordinary events. Communication patterns also change noticeably, with speech becoming disorganized, tangential, or difficult to follow.
Some individuals experience dramatic mood swings, cycling between extreme euphoria, irritability, and profound depression without clear external triggers. Social behaviors typically change markedly, with increasing withdrawal from friends, family, and normal activities as the person becomes more absorbed in their internal experiences and potentially fearful of social interactions.
Many individuals show declining performance in work, school, or other responsibilities as cognitive functions become impaired and attention diverted to internal experiences. Sleep patterns often become significantly disrupted, with insomnia or hypersomnia common as normal circadian rhythms are affected. In some cases, individuals may begin expressing thoughts of harming themselves or others, representing a serious emergency requiring immediate intervention. For more information on cannabis and paranoia, see our article on weed paranoia and psychosis.
Studies have documented that “cannabis can produce a range of acute psychotic symptoms that include depersonalization, derealization, paranoia, ideas of reference, flight of ideas, pressured thought, disorganized thinking, persecutory delusions, grandiose delusions, auditory and visual hallucinations, and impairments in attention and memory” (D’Souza et al., 2009).
The Science Behind Cannabis and Psychosis
Scientific research has established clear connections between cannabis use and psychosis, with multiple studies across different populations consistently finding associations between cannabis consumption patterns and psychotic symptoms. This relationship involves complex interactions between cannabis compounds, genetic vulnerabilities, neurodevelopmental factors, and environmental influences that collectively determine individual risk profiles.
Is There a Dose-Response Relationship?
Research consistently demonstrates a dose-dependent relationship between cannabis and psychosis risk, with higher potency products, more frequent use patterns, and larger consumption amounts all independently increasing the likelihood of psychotic episodes. This relationship follows a clear biological gradient, suggesting a direct causal connection rather than merely an association.
Multiple longitudinal studies tracking cannabis users over time have found that chronic, heavy users of high-potency cannabis have up to five times greater risk of developing psychotic disorders compared to non-users. This dose-response relationship provides some of the strongest evidence for causality in epidemiological research.
Research from the PMC found that “heavy cannabis users of high-potency cannabis have up to five times greater risk of developing psychotic disorders compared to non-users” and that “among each study’s heaviest users, the following longitudinal studies have demonstrated a significantly increased risk of any psychosis outcome” (Radhakrishnan et al., 2014).
How Does Age of First Use Affect Risk?
The timing of cannabis exposure significantly influences its potential psychological impact, with neuroimaging studies confirming that the developing brain—particularly before age 25—shows greater vulnerability to cannabis-related structural and functional changes. During adolescence and early adulthood, the brain undergoes critical periods of development involving pruning of neural connections, myelination of nerve fibers, and refinement of neurotransmitter systems.
Cannabis use during these sensitive periods can potentially disrupt these processes, especially in the prefrontal cortex and limbic regions involved in emotional regulation and reality testing. These neurobiological insights help explain why early-onset cannabis use consistently shows stronger associations with psychosis than adult-onset use.
According to PMC research, “the alleged role played by the endocannabinoid system in late developmental phases such as the adolescent one, prompted speculation that alterations in the endocannabinoid tone induced by cannabis consumption during the adolescent developmental window might represent a risk factor for developing schizophrenia” (Parolaro, 2010).
What Role Do Genetics Play in Cannabis Response?
Genetic factors substantially influence individual responses to cannabis, with specific gene variants related to dopamine regulation, cannabinoid receptor function, and neurodevelopmental processes increasing susceptibility to psychosis. Research in molecular genetics has identified variations in genes like AKT1, COMT, and DRD2 that appear to moderate the relationship between cannabis use and psychosis risk. These genetic factors help explain why only a subset of cannabis users experience psychotic symptoms despite similar consumption patterns.
Ongoing research in pharmacogenetics aims to develop screening tools that could potentially identify individuals at elevated risk before they experience adverse reactions. At Healthy Life Recovery, we integrate genetic understanding through our GeneSight Testing service to better understand how patients metabolize different substances.
Studies have found that “a functional polymorphism of the COMT gene results in two common allelic variants, the valine (Val), and the methionine (Met) allele” and that “in a longitudinal birth cohort study (n > 1,000), adolescents homozygous for the COMT Val108/158Met allele were most likely to exhibit psychotic symptoms or develop schizophrenia if they used cannabis” (D’Souza et al., 2009).
THC vs. CBD: Why Does the Chemical Balance Matter?
The specific chemical composition of cannabis products, particularly the ratio between THC (delta-9-tetrahydrocannabinol) and CBD (cannabidiol), significantly influences psychosis risk. Laboratory and clinical studies demonstrate that THC and CBD have opposing effects on brain function: THC activates cannabinoid receptors in ways that can produce psychotic-like effects, while CBD appears to have antipsychotic properties that may partially counteract THC’s effects. This chemical balance helps explain why traditional cannabis varieties with more balanced THC: CBD ratios appear to carry lower psychosis risk than modern, high-THC strains with minimal CBD content.
This scientific understanding supports harm reduction strategies that emphasize using products with more balanced cannabinoid profiles when cannabis is consumed. For more information on the differences between cannabis compounds, read our article on understanding the difference between THCA & THC.
Research analysis of confiscated cannabis shows that “the mean Δ9-THC:CBD ratio rose substantially from 24.81 in 2009 to 103.48 in 2017” demonstrating a dramatic increase in high-THC, low-CBD products (ElSohly et al., 2021).
What To Do in a Crisis
Responding effectively to a cannabis-induced psychotic episode requires a balanced approach that prioritizes safety while providing appropriate support until professional help can be obtained. These situations can be frightening for everyone involved, but understanding the temporary nature of most cannabis-induced psychotic episodes can help maintain perspective while taking necessary precautions.
How Can You Create a Safe Environment?
Creating a calm, safe environment represents the first critical step when someone appears to be experiencing cannabis-induced psychosis. Reduce environmental stimulation by lowering lights, turning off loud music or television, and moving to a quieter space if possible. Limit the number of people interacting with the affected person to reduce overwhelming social input. Remove potentially dangerous objects from the immediate environment without drawing attention to this action, as this could increase paranoia. The goal is to create conditions that minimize additional stress on an already overloaded nervous system.
When Should You Seek Medical Help?
Seeking appropriate medical help promptly is essential, as cannabis-induced psychosis can occasionally lead to dangerous behaviors or indicate more serious underlying conditions. Call emergency services (911) or transport the person to an emergency room if the situation feels unmanageable or potentially dangerous.
Be prepared to provide medical professionals with specific information about what substances were consumed, including the type of cannabis product, approximate dosage, time of consumption, and whether other substances were also used. This information is critical for proper treatment and will not result in legal consequences for the affected individual in most medical settings, as healthcare providers prioritize patient safety over legal concerns.
How Do You Communicate with Someone Experiencing Psychosis?
While waiting for professional help, maintain a reassuring presence with the person experiencing psychosis.
• Stay with them continuously, as abandonment can significantly worsen paranoia and anxiety.
• Speak clearly in short, simple sentences using a calm, reassuring tone.
• Avoid whispering to others or having side conversations that could be misinterpreted as threatening.
• Maintain a non-threatening body posture and appropriate distance to avoid triggering fear responses.
• If the person is experiencing hallucinations or delusions, neither directly challenge nor reinforce these perceptions. Instead, acknowledge their distress without confirming or disputing the content of their experiences with responses like “That sounds frightening” rather than “That’s not real.”
Remember that argumentative approaches typically increase distress and can potentially escalate the situation. Focus instead on providing reassurance that the experience is temporary and help is coming. If the situation involves a dual diagnosis with other mental health conditions, learn more about our dual diagnosis treatment approach.
Getting Help for Cannabis Use Disorder
Cannabis use disorder affects approximately 9% of people who use cannabis, with rates rising to about 17% for those who begin using during adolescence. This condition involves problematic patterns of use leading to clinically significant impairment or distress, often manifesting as difficulty controlling consumption despite negative consequences. If you’ve experienced cannabis-induced psychosis yet find yourself continuing to use, or if you’ve developed patterns of use that differentiate between dependence vs. addiction, effective treatment options exist that can help you regain control and address underlying issues.
When Should You Talk to a Healthcare Provider?
In the 1970s, the average THC content in cannabis samples was approximately 2%, creating a relatively mild psychoactive experience by today’s standards. Most cannabis available during this era was imported as less potent mixtures of leaves, stems, and flowers.
By the 1990s, as domestic cultivation increased and growing techniques improved, average THC concentrations had doubled to around 4-5%, still modest compared to current products. Today’s commercially grown cannabis flowers regularly test between 15-25% THC, representing a five to ten-fold increase over what was available just a few decades ago. This dramatic escalation continues with modern concentrates, which can range from 40% to nearly pure THC at 99%, creating products with unprecedented potency in human history.
According to research published by the National Institutes of Health, “the mean Δ9-THC concentration has increased over the last 10 years, from 9.75% in 2009 to 14.88% in 2018 and 13.88% in 2019” (ElSohly et al., 2021). NIDA reports that “between 1995 and 2022 the delta-9 THC potency (strength) in illegal cannabis products seized by law enforcement quadrupled from 3.96% to 16.14%” (NIDA, 2024).
When Should You Talk to a Healthcare Provider?
Beginning a conversation about cannabis concerns with a trusted healthcare provider creates an important foundation for recovery. Primary care physicians, psychiatrists, or addiction specialists can evaluate symptoms, assess for co-occurring conditions, and recommend appropriate treatment pathways. Many providers now take a non-judgmental approach to cannabis use disorders, recognizing them as medical conditions rather than moral failings. This initial conversation can help determine whether outpatient treatment, intensive outpatient programs, or residential treatment would best suit your specific situation.
Some providers may recommend medication options to manage withdrawal symptoms or address underlying conditions like anxiety or depression that might contribute to problematic cannabis use. Our outpatient rehab programs are designed to accommodate various levels of need.
What Therapeutic Approaches Work for Cannabis Use Disorder?
Evidence-based psychotherapeutic approaches show significant effectiveness for cannabis use disorders. Cognitive Behavioral Therapy (CBT) helps identify and modify thought patterns and behaviors associated with cannabis use while developing coping skills for triggers and cravings. Motivational Enhancement Therapy (MET) explores ambivalence about changing cannabis use patterns and strengthens motivation for positive change. Contingency Management provides tangible rewards for achieving treatment goals and maintaining abstinence. These approaches can be delivered individually or in group settings, with research suggesting that a combination of approaches often yields the best outcomes. Many people also benefit from family therapy, particularly when family dynamics influence use patterns or when family support would strengthen recovery efforts.
How Can Healthy Life Recovery Help with Cannabis Concerns?
At Healthy Life Recovery, we understand the complex nature of cannabis use disorders and provide comprehensive treatment options that address both the psychological and physical aspects of dependence.
Our programs incorporate evidence-based approaches tailored to individual needs, with specialized attention to cannabis-induced psychosis and co-occurring mental health conditions. Our treatment team includes addiction specialists familiar with the unique challenges of cannabis dependence in today’s high-potency landscape. We offer multiple levels of care, from intensive outpatient programming to comprehensive aftercare planning, providing the structure and support needed for sustainable recovery from cannabis use disorder.
The Bottom Line
The cannabis landscape has transformed dramatically in recent decades, creating new challenges for public health, medical providers, and consumers. This evolution from relatively mild plant material to highly engineered products with unprecedented potency demands a parallel evolution in how we understand and discuss cannabis risks. As we approach 4/20, a day traditionally celebrating cannabis culture, it’s particularly important to foster nuanced conversations about these changing risk profiles.
Making informed health decisions requires accurate, non-biased information about potential risks without exaggeration or minimization. While many people use cannabis without experiencing psychosis or other significant adverse effects, acknowledging the real risks associated with high-potency products represents an essential aspect of responsible use. This balanced perspective recognizes both the therapeutic potential of cannabis for some conditions and the legitimate concerns about its potential psychological impacts, particularly in vulnerable populations. As cannabis continues its trajectory toward mainstream acceptance, this nuanced understanding becomes increasingly important for both individual health decisions and public policy considerations.
If you or someone you know has experienced cannabis-induced psychosis or struggles with problematic cannabis use patterns, professional support can make a significant difference in recovery outcomes.
At Healthy Life Recovery, our comprehensive approach addresses both the immediate concerns related to cannabis use and the underlying factors that may contribute to substance use disorders. Our evidence-based addiction treatment programs provide the structure, support, and clinical expertise needed to navigate the challenges of cannabis dependence in today’s high-potency landscape. Please reach out to Healthy Life Recovery at (844) 252-8347 or contact us to learn more about how our specialized programs can support your journey toward recovery and wellness.

Medically Reviewed By:
Dr. Sanjai Thankachen
Dr. Sanjai Thankachen graduated from Adichunchanagiri Institute of Medicine in 2000. He completed his residency in psychiatry in 2008 at Creedmoor Psychiatric Center in New York. Dr. Thankachen is currently working with Pacific Neuropsychiatric Specialists in an outpatient practice, as well as working at multiple in-patient psychiatric and medical units bringing his patients the most advanced healthcare treatment in psychiatry. Dr. Thankachen sees patients with an array of disorders, including depression, bipolar illness, schizophrenia, anxiety, and dementia-related problems.

Edited for Clinical Accuracy By:
Sean Leonard, Psychiatric Nurse Practitioner
Sean Leonard is a board-certified psychiatric nurse practitioner. He received his master’s degree in adult geriatric primary care nurse practitioner from Walden University and a second postmaster specialty in psychiatry mental health nurse practitioner from Rocky Mountain University. Sean has experience working in various diverse settings, including an outpatient clinic, inpatient detox and rehab, psychiatric emergency, and dual diagnosis programs. His specialty areas include substance abuse, depression, anxiety, mood disorders, PTSD, ADHD, and OCD.
