Medication-Assisted Treatment For Opioid Use Disorder

Table of Contents
What Is OUD?
Opioids1 are prescribed by doctors primarily to treat pain. When used in the long-term, though, a decrease in pain-relieving effects can be experienced, and pain can gradually progress.
Opioid use disorder (OUD) can develop very suddenly, and dependence on the drug can form even when the opioid is appropriately used, as the doctor prescribed. Nearly all prescription opioids cause withdrawal symptoms, which creates great difficulty when attempting to stop taking them.
Indicators of possible addiction can be seen when the user’s daily routines and mental health become compromised. By taking more than the prescribed amount, the probability of dependence is increased significantly. These substance use disorders often lead to an opioid overdose, which is known to result in death.
Signs & Symptoms of OUD
The struggle with opioid use disorder does not always display visible symptoms right away. However, it is crucial that when the signs or symptoms do appear, they are recognized as soon as possible so that the dangerous addiction can be addressed.
Some common signs and symptoms have been seen to include:The struggle with opioid use disorder does not always display visible symptoms right away. However, it is crucial that when the signs or symptoms do appear, they are recognized as soon as possible so that the dangerous addiction can be addressed.
Some common signs and symptoms have been seen to include:
Frequent flu-like symptoms
Weight loss
Newer financial issues
Isolation from friends and family members
Intense cravings or urges for the opioid drug
Withdrawing from previously enjoyed activities
Having frequent doctor visits
Inconsistent sleeping habits
Sudden dramatic mood swings
Trouble staying awake
How Opioids Became So Deadly
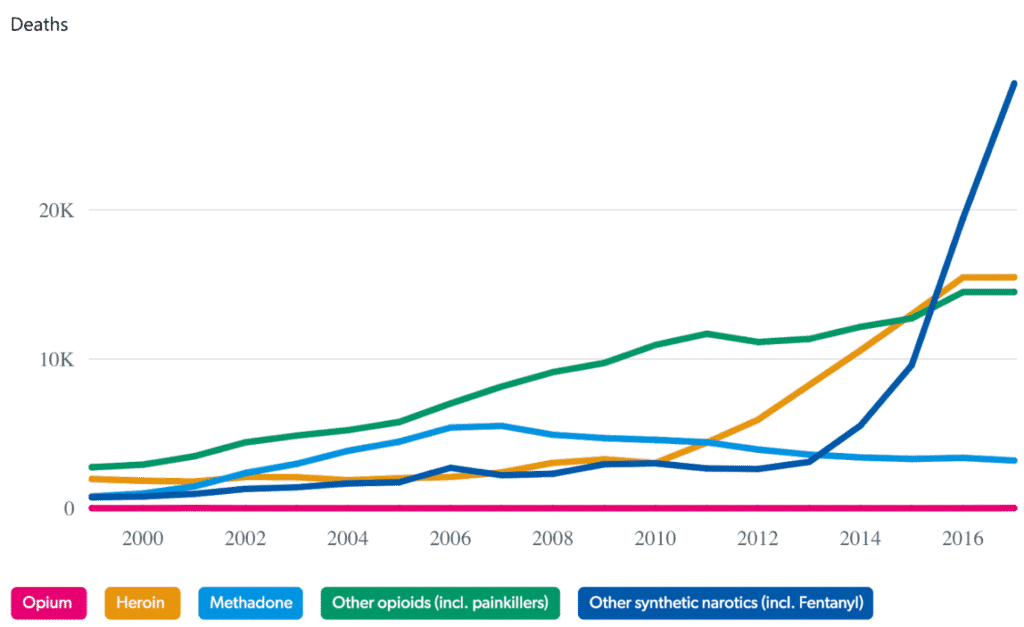
Deaths from various opioids and synthetics like heroin, fentanyl, and prescription painkillers have all increased since 2013.
Fentanyl is a very potent pain medication that is up to 100 times stronger than morphine. The tremendous strength of this drug stands out because there has been an estimated 800% increase in fatalities from an overdose in just four short years. Since each individual may be affected differently, the drug creates very unpredictable outcomes. Many people can find that even a tiny dose of fentanyl to be deadly.
In the year 2017 alone, opioids were solely responsible for 46,394 deaths from overdose.
- This statistic has gotten a lot of attention because it’s nearly double the number of deaths caused by non-opioid substances
What is MAT?
Medication-assisted treatment (MAT) is a practical evidence-based treatment approach in opioid Treatment Programs,2 (OTPs) provided by qualified treatment facilities throughout the United States. The appropriate use of specialized counseling and behavioral therapies is the perfect evidence-based combination proven to save lives and significantly increase the recovery rates.
Everyone seeking treatment for an opioid use disorder should be offered access to all of the approved medication options to assist in the recovery process. This allows addiction specialists or other medical professionals to work with patients individually to select the treatment that proves to be the best fit for their needs.
Due to the persistent and deep-rooted nature of addiction, the demand for extended services like MAT for opioid treatment should be re-examined periodically. There is not a current recommendation for the duration treatment . In some cases19, it has become the best and safest option for the patient’s treatment to continue indefinitely.
Medications
Methadone3
By being characterized as a full agonist, this drug primarily works with both the nervous system and brain receptors to produce positive results. This combination in methadone is designed to ease opioid withdrawal symptoms and also to block the euphoric effects that come from most opioid drugs. The side-effects of taking methadone are minimal when the drug is administered correctly.
Suboxone4
This drug is made with a combination of buprenorphine and naloxone.
Similar to methadone, suboxone is a partial agonist. So instead of being the primary function, this drug binds to the brain and nervous system receptors too, but only partially. Treatment patients taking suboxone for opioid addiction typically report a decrease in craving intensity, as well as physical symptoms, becoming alleviated.
Vivitrol5
This FDA-approved medication is an injectable naltrexone-based drug that only needs to be administered once a month. The use of Vivitrol, however, requires whoever is taking it to abstain from taking any other opioid for at least 14 days before the treatment and injections can begin. The primary purpose of Vivitrol is to decrease or eliminate the cravings for extended periods significantly.
Sublocade6
Sublocade is most commonly used in treatment where there was evidence of abuse using prescription painkillers such as morphine, oxycodone, and fentanyl. This drug has also been seen to be effective when treating heroin addictions, and like Vivitrol, it is administered just one time per month.
MYTH vs. FACT
Myth:
Risk of overdose increases for MAT patients.
Fact:
If anything, medication-assisted treatment programs help to prevent overdoses rather than increase the chances of them occurring. It’s vital to note that even a single dose of opioids after a full detox has proven to be life-threatening and cause fatal overdoses.
Myth:
MAT programs are only successful short-term
Fact:
Studies have shown that patients participating in MAT-style programs for at least 1-2 years have shown to have the highest rates of achieving long-term success7. There is currently no compelling evidence that indicates that there would be multiple benefits from eliminating MAT programs.
Myth:
MAT programs prolong the recovery process
Fact:
Recent recovery rates show that medication-assisted treatment practices have been more often than not, providing patients the help and guidance necessary to make consistent progress10. Improving the level of basic functionality, the ability to handle stress, and developing a stable overall quality of life.Myth:
Self-control is better than MAT
Fact:
MAT practices are continually being improved upon based on the evidence seen throughout the patient’s treatment and recovery. MAT has considered being among the most reliable rehabilitation processes and receives more recommendations than any other treatment option when treating opioid addiction.
Myth:
MAT is NOT covered by insurance
Fact:
As of May 2013, Medicaid FFS programs agreed to cover maintenance treatment with methadone in 31 states. This coverage was said to be provided while participating in opioid addiction treatment programs8. Medicaid agencies vary when it comes to buprenorphine being listed on the Preferred Drug List (PDL), while naltrexone is listed on the Medicaid PDL in over 60% of US states9.
Notable recommendations are from:
Opioid MAT Effectiveness: What Is The Data?
The alarming increases in opioid supply are being pushed by both legal prescriptions written by qualified professionals, as well as illegally trafficked from around the world. The painkiller availability peak hit in 2012, where data16 showed an estimated 81 per 100 people17 receiving prescriptions.
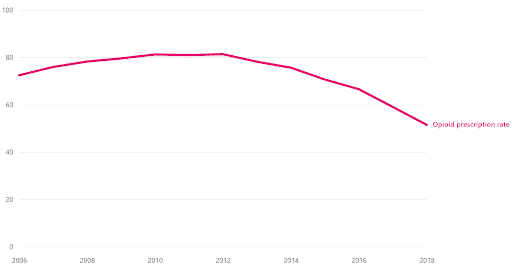
This is given a lot of attention in an attempt to significantly decrease the numbers in the near future
Many efforts including the development of newly controlled state-wide regulations18 are being organized and implemented
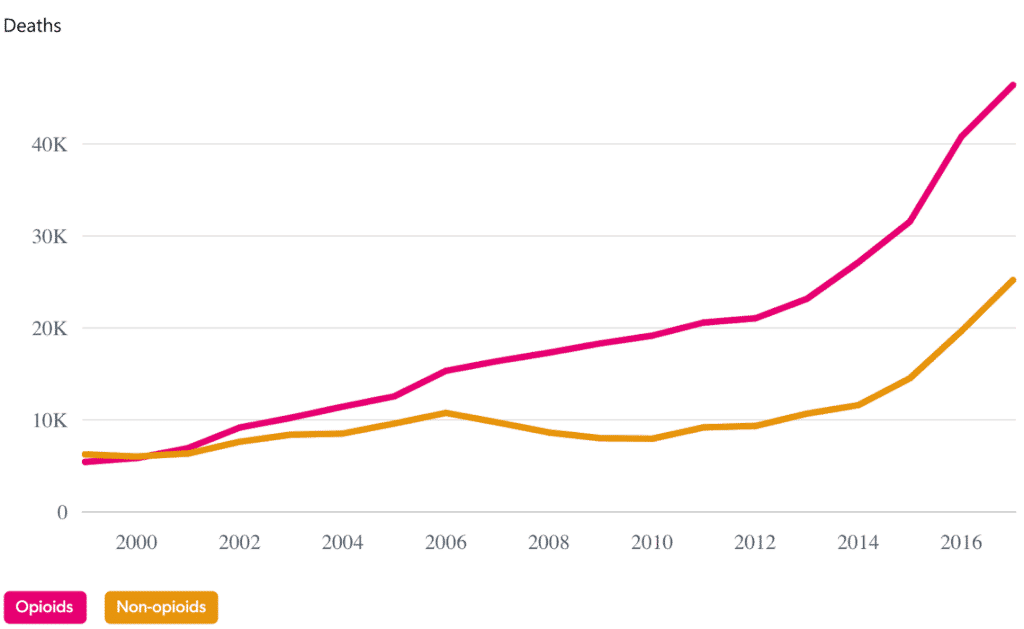
Opioids are responsible for more fatalities than cars or guns and nearly the same as annual suicides in the United States

Medically Reviewed By:
Dr. Sanjai Thankachen
Dr. Sanjai Thankachen graduated from Adichunchanagiri Institute of Medicine in 2000. He completed his residency in psychiatry in 2008 at Creedmoor Psychiatric Center in New York. Dr. Thankachen is currently working with Pacific Neuropsychiatric Specialists in an outpatient practice, as well as working at multiple in-patient psychiatric and medical units bringing his patients the most advanced healthcare treatment in psychiatry. Dr. Thankachen sees patients with an array of disorders, including depression, bipolar illness, schizophrenia, anxiety, and dementia-related problems.

Edited for Clinical Accuracy By:
Sean Leonard, Psychiatric Nurse Practitioner
Sean Leonard is a board-certified psychiatric nurse practitioner. He received his master’s degree in adult geriatric primary care nurse practitioner from Walden University and a second postmaster specialty in psychiatry mental health nurse practitioner from Rocky Mountain University. Sean has experience working in various diverse settings, including an outpatient clinic, inpatient detox and rehab, psychiatric emergency, and dual diagnosis programs. His specialty areas include substance abuse, depression, anxiety, mood disorders, PTSD, ADHD, and OCD.
Resources
- Geneen, L. J., Moore, R. A., Clarke, C., Martin, D., Colvin, L. A. & Smith, B. H. (2017). Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database of Systematic Reviews, 2017(4): CD011279.
- Non-opioid treatment. (n.d.). Retrieved December 21, 2019 from https://www.asahq.org/whensecondscount/pain-management/non-opioid-treatment/
- Therapeutic massage for pain relief. (2016, July). Retrieved December 21, 2019 from https://www.health.harvard.edu/alternative-and-complementary-medicine/therapeutic-massage-for-pain-relief
- Yoga for pain relief. (2015, April). Retrieved December 21, 2019 from https://www.health.harvard.edu/alternative-and-complementary-medicine/yoga-for-pain-relief
- Lim, J. A.C., Choi, S. H., Lee, W. J., Jang, J. H., Moon, J. Y., Kim, Y. C., & Kang, D. H. (2018, June). Cognitive-behavioral therapy for patients with chronic pain. Medicine (Baltimore), 97(23): e10867.
- Elkins, G., Jensen, M. P., & Patterson, D. R. (2009). Hypnotherapy for the management of chronic pain. International Journal of Clinical and Experimental Hypnosis, 55(3): 275-287.
- Chen. W. G. (2016). Mindfulness meditation reduces pain, bypasses opioid receptors. Retrieved December 21, 2019 from https://nccih.nih.gov/research/blog/mindfulness-meditation-pain
- Mehlsen, M., Heegarrd, L. & Frostholm, L. (2015). A prospective evaluation of the Chronic Pain Self-Management Programme in a Danish population of chronic pain patients. Patient Education and Counseling. 98(5): 677-680.
- Non-opioid treatment. (n.d.). Retrieved December 21, 2019 from https://www.asahq.org/whensecondscount/pain-management/non-opioid-treatment/
- Hansen, G. R. & Streltzer, J. (2005). The psychology of pain. Emergency Medical Clinics of North America, 23(2005): 339-348.
- Non-opioid treatment. (n.d.). Retrieved December 21, 2019 from https://www.asahq.org/whensecondscount/pain-management/non-opioid-treatment/
- Abdallah, C. G. & Geha, P. (2017). Chronic pain and chronic stress: two sides of the same coin? Chronic Stress. Retrieved December 22, 2019 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5546756/
- Pain and sleep. (n.d.). Retrieved December 22, 2019 from https://www.sleepfoundation.org/articles/pain-and-sleep
- Can diet heal chronic pain? (2018, July). Retrieved December 22, 2019 from https://www.health.harvard.edu/pain/can-diet-heal-chronic-pain
